Basics
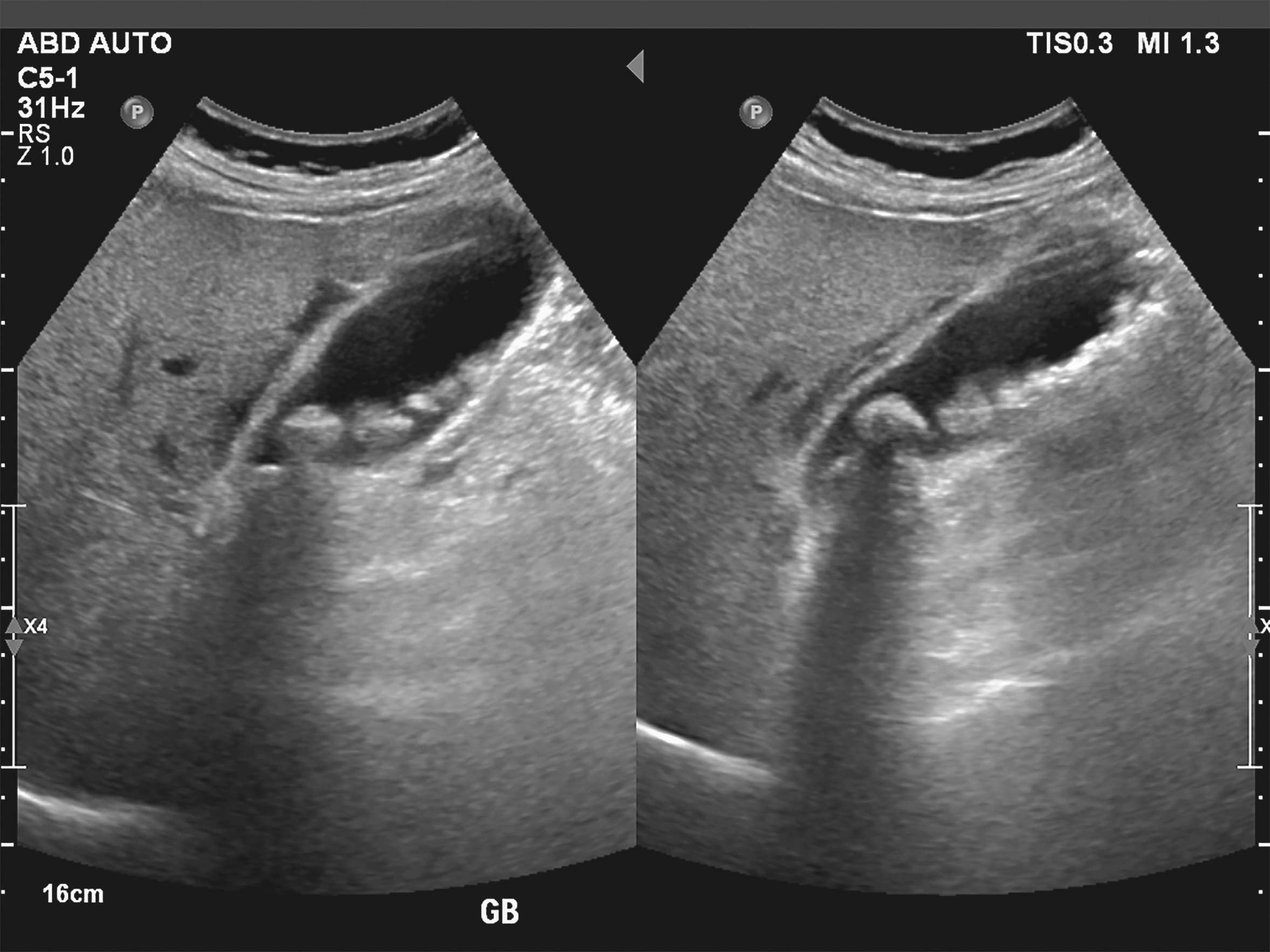
The term cholelithiasis refers to the presence of gallstones. These can occur either in the gallbladder (cholecystolithiasis), the bile ducts (choledocholithiasis) or in the small bile ducts of the liver (cholangiolithiasis). Around 10 to 15 % of the population have gallstones, although most of those affected remain symptom-free. Small gallstones are also often referred to as bile sand, sludge or gallstones.
The human body produces around 700 ml of yellow-brown to olive-green bile per day, which enables (fat) digestion in the small intestine. This consists of
Water (82 %)
electrolytes
Bile acids (subject to the enterohepatic circulation)
Phospholipids (especially lecithin)
cholesterol
bilirubin
proteins
The most common forms of gallstones are cholesterol, pigment and mixed gallstones. Cholesterol stones and mixed gallstones together account for around 80 % of gallstones in industrialized countries. Pigment stones account for around 20% of gallstones.