Drug therapy
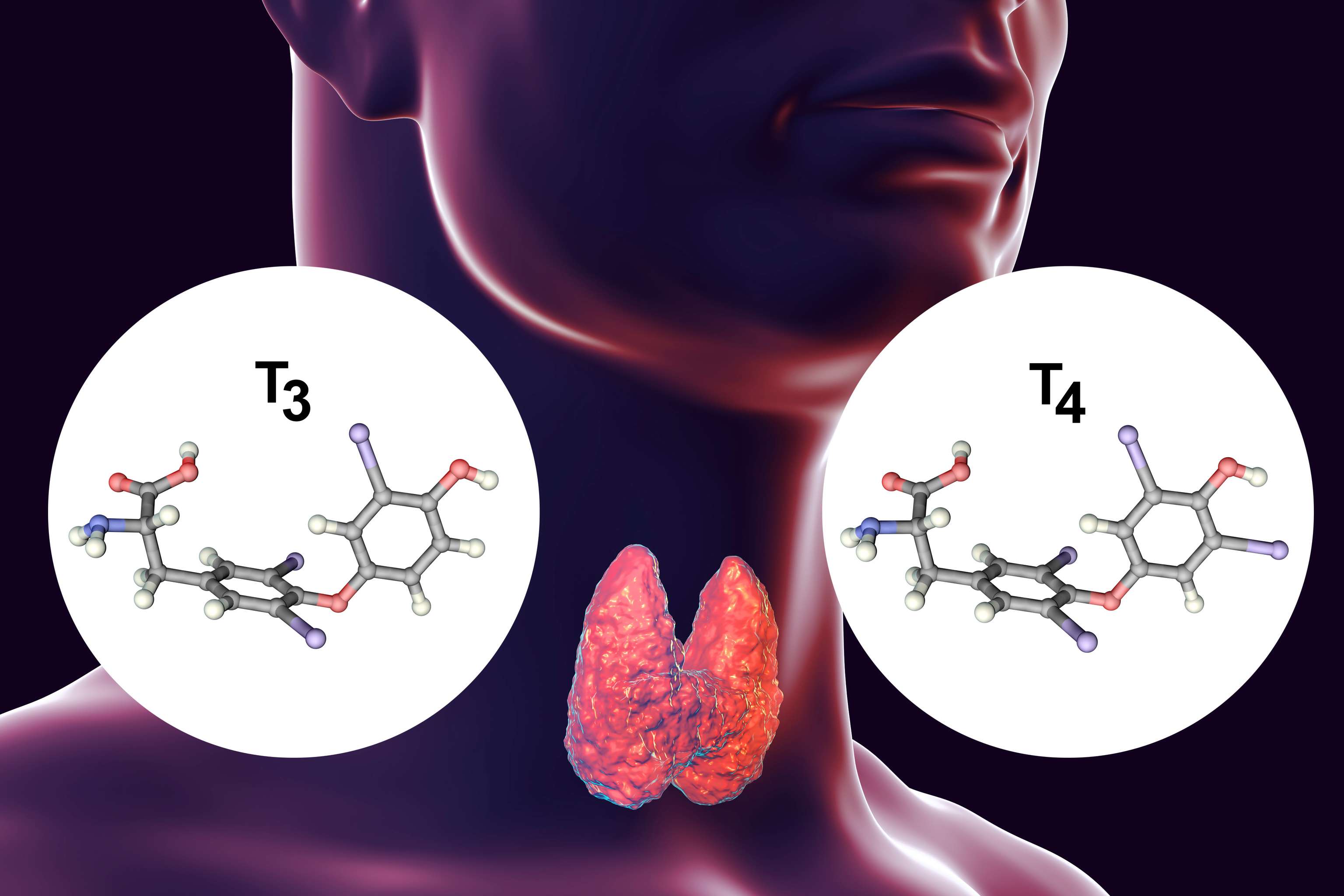
Treatment is usually medicinal with thyrostatic drugs. Thyreostatics inhibit hormone production and release in the thyroid gland. Thiamazole or carbimazole (precursor of thiamazole) is the drug of choice here; propylthiouracil can also be used as an alternative. Beta-blockers such as propanolol are also given for symptomatic treatment of tachycardia. Propanolol also inhibits the enzyme deiodinase and thus the conversion of the thyroid hormone T4 to the metabolically active T3. As with any hyperthyroidism, treatment with thyrostatic agents should continue until euthyroidism (good thyroid function) is achieved. In Graves' disease, thyrostatic therapy normally lasts 1-1.5 years, in individual cases even longer.
About 6 months after diagnosis or start of therapy, the TRAK level in the blood is checked. This has prognostic significance: at levels > 10 IU/l, the probability that the therapy will still be effective or that the disease will subside is reduced. In this case, the thyroid gland is switched off by radioiodine therapy or surgically removed.
After discontinuation of medication, recurrence (recurrence of the disease) occurs in about 50% of cases, but usually thyroid function normalizes in more than half of patients. Smoking increases the risk of recurrence and worsens ocular involvement in Graves' disease.
In case of non-improvement or recurrence of hypothyroidism after 1-1.5 years of thyrostatic therapy, permanent elimination of the thyroid gland by radioiodine therapy or surgical removal is indicated.
Radioiodine therapy
In radioiodine therapy, radioactive iodine is taken orally, which accumulates in the thyroid gland and destroys the hormone-producing cells. The thyroid gland should be treated in advance with thyrostatic drugs, which are discontinued 2-3 days before radioiodine therapy. In addition, a low iodine diet should be followed and iodine-containing drugs or supplements should be avoided. Since the effect radioiodine therapy occurs only after a few weeks, follow-up treatment with thyrostatic drugs may also be necessary. Hypothyroidism may worsen an existing endocrine orbitopathy (inflammatory disease of the orbits) and should be prevented. Therefore, at the beginning of the onset of action of radioiodine therapy, thyrostatic medication can be combined early with levothyroxine (LT4). Short-term and regular monitoring of thyroid parameters after radioiodine administration is therefore essential. Once thyroid function has been permanently abolished, lifelong thyroid hormone(LT4) substitution is necessary.
Surgical therapy
Surgical removal of the thyroid gland is an alternative to radioiodine therapy. Surgery for Graves' disease is indicated primarily in cases of uncontrolled thyroid growth, endocrine orbitopathy, suspected malignant change in the thyroid gland, severe side effects and intolerance of threostatic drugs, or if the patient refuses radioiodine therapy. Prior to surgery, good thyroid function should always be achieved by thyrostatic pretreatment. In Graves' disease, the entire thyroid gland is usually removed except for a remnant of 2 ml (so-called fast-total thyroidectomy). During surgery, there is a risk of injury to the vocal cord nerve, which can lead to paralysis of the vocal cords and subsequently to temporary to lifelong hoarseness. Thyroid surgery may also cause short-term damage to the parathyroid glands, which are responsible for maintaining blood calcium levels. In this case, calcium must be taken for a few days after surgery, and if the parathyroid glands are permanently damaged, patients must rely on lifelong calcium intake in combination with vitamin D. Even after thyroid removal, thyroid hormone tablets(LT4) must be taken for life and thyroid parameters must be monitored at regular intervals.
Treatment of eye symptoms
For the treatment of the typical eye symptoms, there are the following options, depending on the auprimation:
- Tablets or infusions with cortisone.
- Selenium substitution in mild cases
- Eye drops, ointments and gels for dry eyes
- Irradiation of the eye socket (in severe cases)
- Surgery (to enlarge the eye socket, in severe cases)