Basics
In the case of high blood pressure (arterial hypertension), the values of the measurable blood pressure are elevated over a longer period of time. The medical term arterial hypertension is made up of the Latin words "arterial" (belonging to the artery) and "hypertension" (excess pressure). According to the current guidelines of the European Society of Cardiology (ESC), we speak of high blood pressure if the systolic blood pressure values exceed 140 mmHg (millimeters of mercury) or the diastolic values exceed 90 mmHg. Arterial hypertension is the most common internal disease and is one of the classic widespread diseases, with the prevalence of hypertension in adults in Europe being around 30%. The prevalence of high blood pressure also depends on body weight, socio-economic status and gender - men are more frequently affected by high blood pressure overall.
Systolic and diastolic values
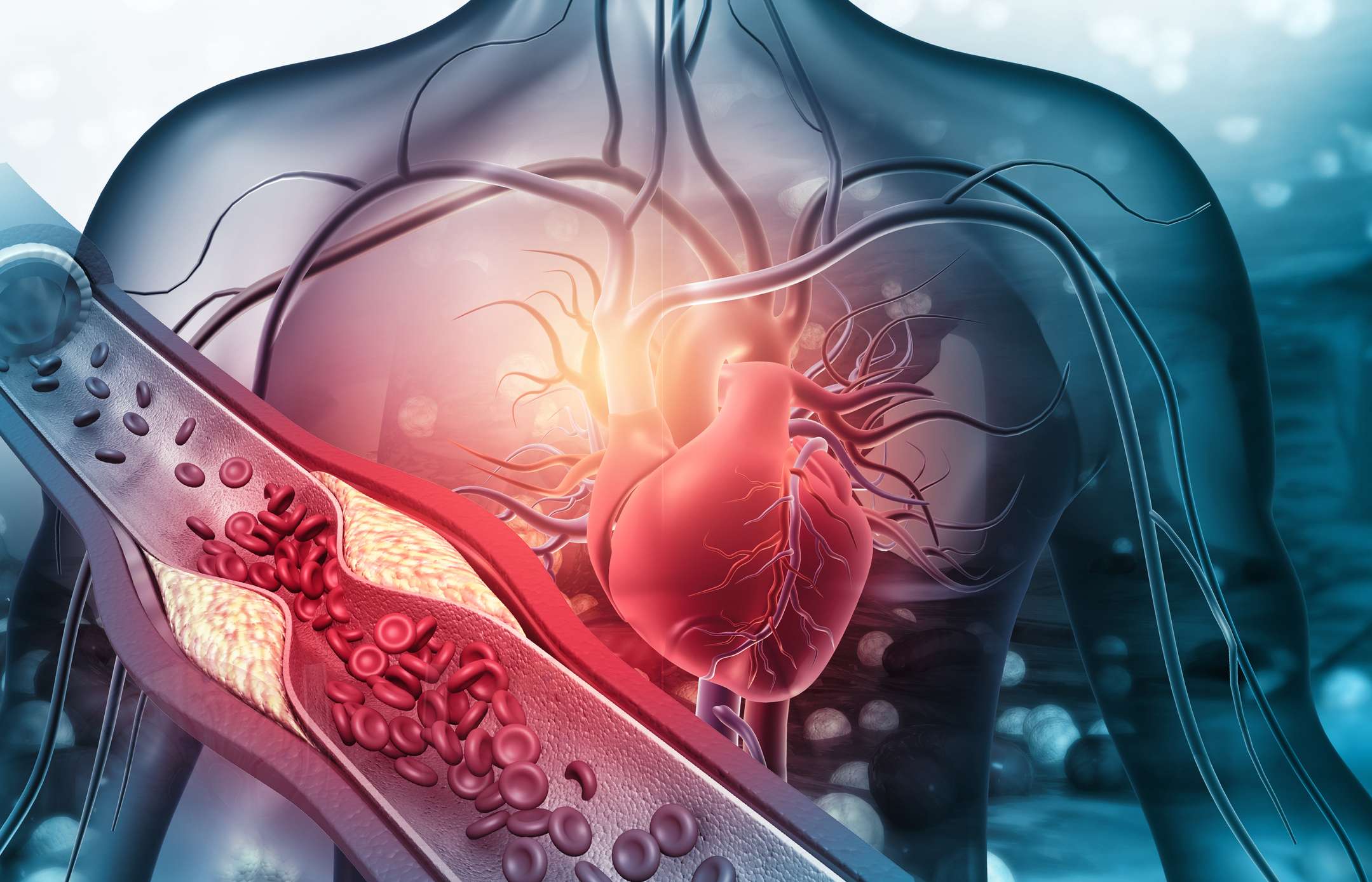
The heart pumps blood into the body with every beat, creating a pressure within the blood vessels that can be measured using a blood pressure cuff, for example. The ideal blood pressure value is 120 / 80 mmHg. The first, usually higher value, is called systolic blood pressure and the second, usually lower value, is called diastolic blood pressure. Systole is the phase in which the heart muscle contracts and ejects blood from the left ventricle. This is contrasted with diastole, in which the heart relaxes and can therefore refill with blood. Blood pressure is usually measured using a blood pressure cuff on the upper arm or invasively using a sensor in the arteries. The blood pressure cuff should always be placed at the level of the heart during a measurement.
The unit for blood pressure is, for historical reasons, mmHg. This stands for millimeters of mercury. High blood pressure is defined as blood pressure above 140 mmHg in systole or above 90 mmHg in diastole.
A one-off moderately high blood pressure often poses no acute danger, but high blood pressure values over a longer period of time have negative effects on the heart, blood vessels, kidneys, eyes and brain. It also increases the risk of cardiovascular diseases such as heart attacks and strokes. This risk can be significantly reduced by treating high blood pressure.
Cardiovascular risk
Whether and how arterial hypertension needs to be treated depends on the blood pressure measured and also on the overall risk of cardiovascular disease. Other diseases such as metabolic syndrome, elevated blood lipids (dyslipidemia) and diabetes mellitus can also increase the cardiovascular risk. A categorical classification of the overall cardiovascular risk is therefore recommended. In Europe, the tool of the European Society of Cardiology (ESC) or the PROCAM health test is recommended for this purpose, which takes into account factors such as systolic blood pressure, gender, smoking habits, age and blood lipid values. These can be used to classify patients into groups according to the calculated risk. According to the ESC recommendations, cardiovascular risk is classified using the SCORE system, for example.
General table of systolic and diastolic blood pressure values:
Designation | systolic in mmHg | diastolic in mmHg |
|---|---|---|
| Optimal | < 120 | < 80 |
| Normal | 120 - 129 | 80 - 84 |
| High normal | 130 - 139 | 85 - 89 |
| Grade 1 hypertension | 140 - 159 | 90 - 99 |
| Grade 2 hypertension | 160 - 179 | 100 - 109 |
| Grade 3 hypertension | ≥180 | ≥ 110 |
| Isolated systolic hypertension | ≥140 | < 90 |
Blood pressure values of over 180/110 mmHg (grade 3) with evidence of acute organ damage are defined by the ESC as a hypertensive emergency. This requires immediate medical treatment.
A condition with blood pressure values of over 180/110 mmHg without organ damage but with additional symptoms is also known as a hypertensive crisis.
The term hypertensive derailment is also widely used and usually describes high blood pressure values in the sense of a grade 3 without symptoms or organ damage.
However, the terms hypertensive crisis and hypertensive derailment are not uniformly defined and are also used differently.