Meningitis is often diagnosed with the help of a detailed medical history, a physical examination, a cerebrospinal fluid puncture, a blood test and various imaging procedures (e.g. computer tomography or magnetic resonance imaging). With the help of computer tomography (CT), for example, complications (e.g. brain abscesses) can be quickly identified and, if necessary, treated.
During a lumbar puncture (cerebrospinal fluid puncture), cerebrospinal fluid is removed from the patient's spinal canal using a cannula. These samples can then be further examined for various pathogens and signs of inflammation.
The blood test for meningitis usually includes a bacterial culture, a complete blood count, signs of inflammation, glucose and possibly other laboratory values. In the case of bacterial meningitis, the blood count often shows an increase in white blood cells (leukocytosis) and an increase in C-reactive protein (CRP). A procalcitonin determination can help to differentiate between bacterial and viral meningitis.
Bacterial meningitis can also lead to hearing and balance disorders, which can be checked using audiometric hearing tests, auditory evoked potentials (brainstem audiometry, AEP) and balance tests.
Common pathogens
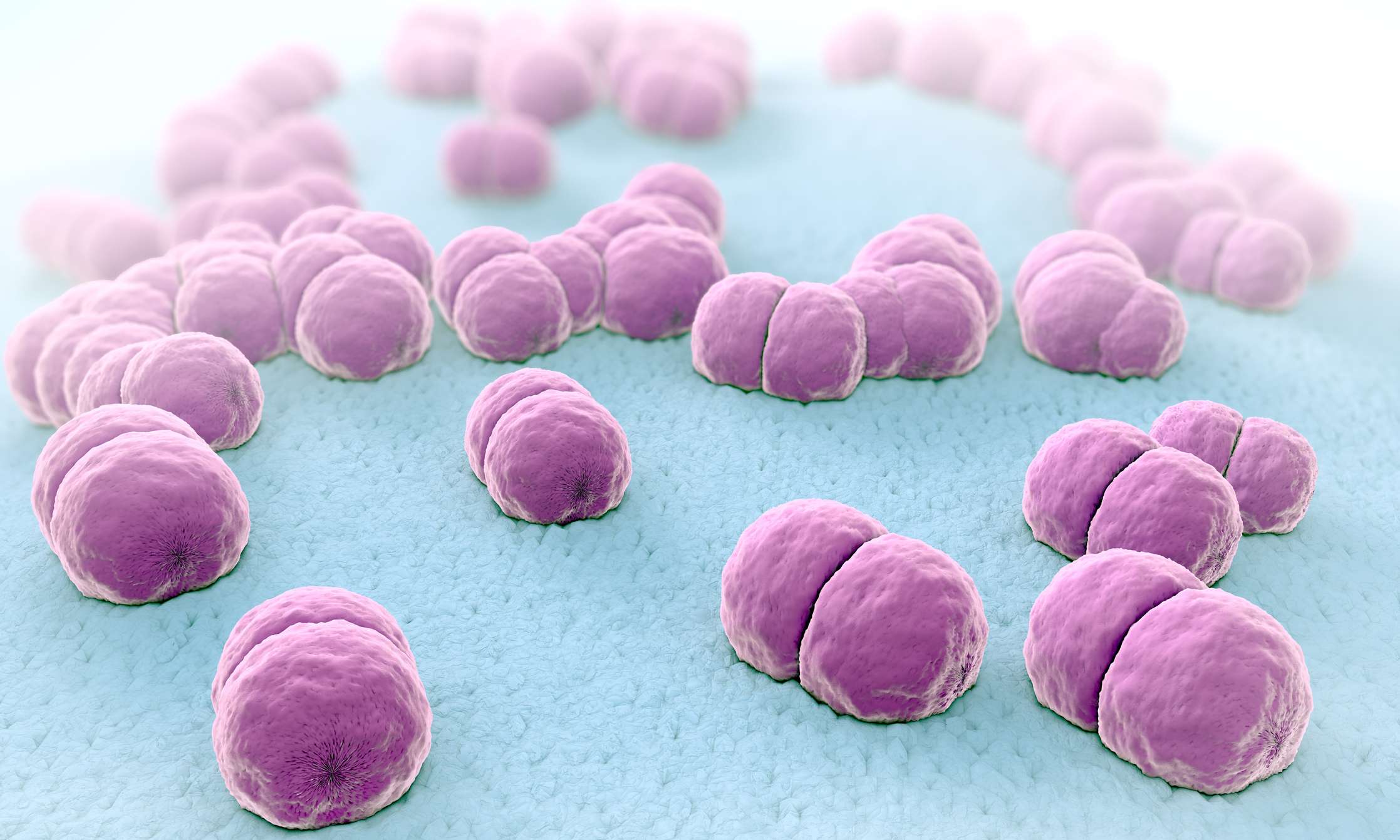
The most common pathogens causing bacterial meningitis in adults and children are pneumococci and meningococci. Rarer pathogens are listeria (< 5 %), staphylococci (< 5 %) and pseudomonads or gram-negative enterobacteria. Due to the high vaccination rate of children against H. influenzae, Haemophilus meningitis has become much rarer than in the past.
In newborns, around 70 % of meningitis is caused by group B streptococci. Various mixed infections with different pathogens can occur, particularly in patients with immune deficiencies (e.g. HIV, leukemia, various immunodeficiencies) or after open craniocerebral trauma. Splenectomies lead to an increased risk of meningitis caused by pneumococci, meningococci and H. influenzae.