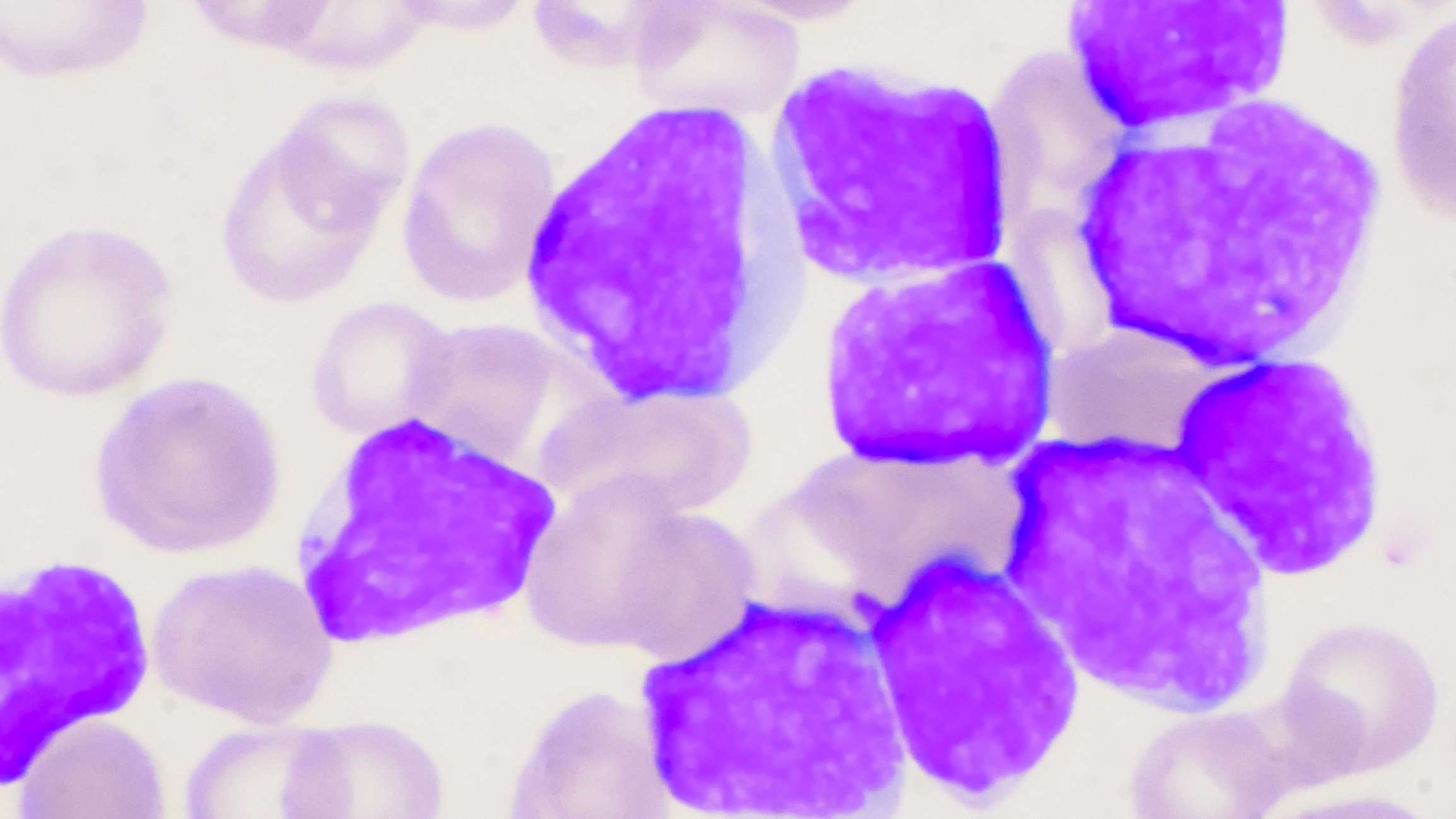
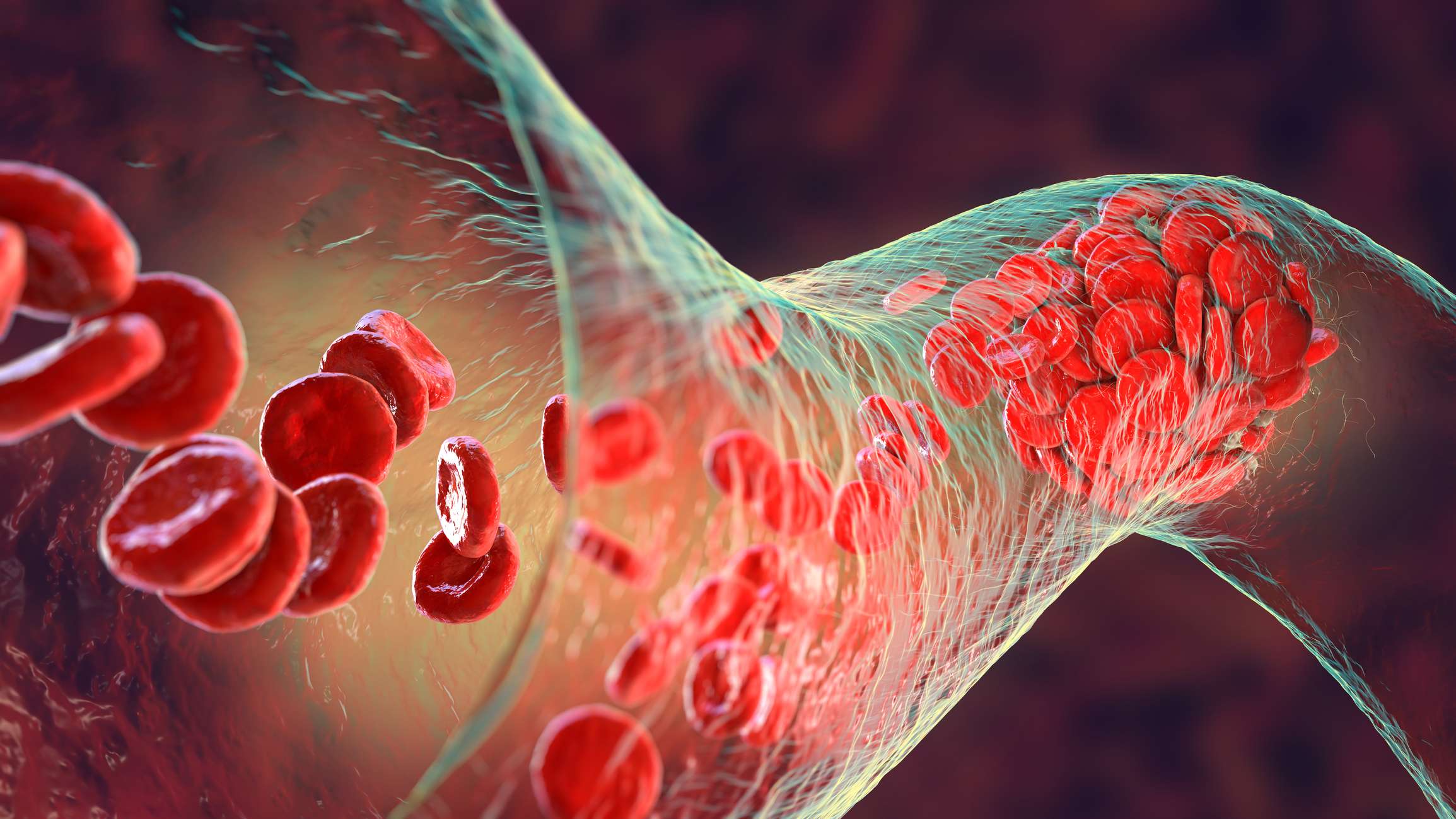
Thrombotic thrombocytopenic purpura, like hemolytic uremic syndrome (HUS), is a so-called thrombotic microangiopathy. Here, the formation of blood clots leads to a disturbance of the blood flow in the smallest blood vessels. This disruption then leads to an oxygen deficiency in the organs supplied (e.g. kidney or brain). The most common form of TTP is the acquired form (about 95% of cases). This is triggered by antibodies against the metalloprotease that normally cleaves von Willebrand factor (ADAMTS 13). The protease ADAMTS 13 plays a major role in the coagulation cascade, with a deficiency leading to an increased incidence of blood clots.
The following causes are possible for acquired TTP:
The congenital form of TTP is also known as Upshaw-Schulman syndrome or cTTP ("congenital TTP"). It is responsible for about 5% of all cases of the disease and often occurs in early childhood (about 50-60% of cases). However, some patients become symptomatic only at the age of 30 - 40 years. cTTP is due to a congenital reduction in ADAMTS13 activity, with over 100 responsible mutations currently known. In most cases, a decrease in ADAMTS 13 activity or decreased secretion of metalloprotease triggers the disease.
Possible triggers for a cTTP flare include:
Trigger
The causes of acquired TTP or of a disease flare-up in the course of TTP are usually influenza or gastrointestinal infections. In addition, drugs such as quinine, Tiklyd or mitomycin can trigger TTP.