Basics
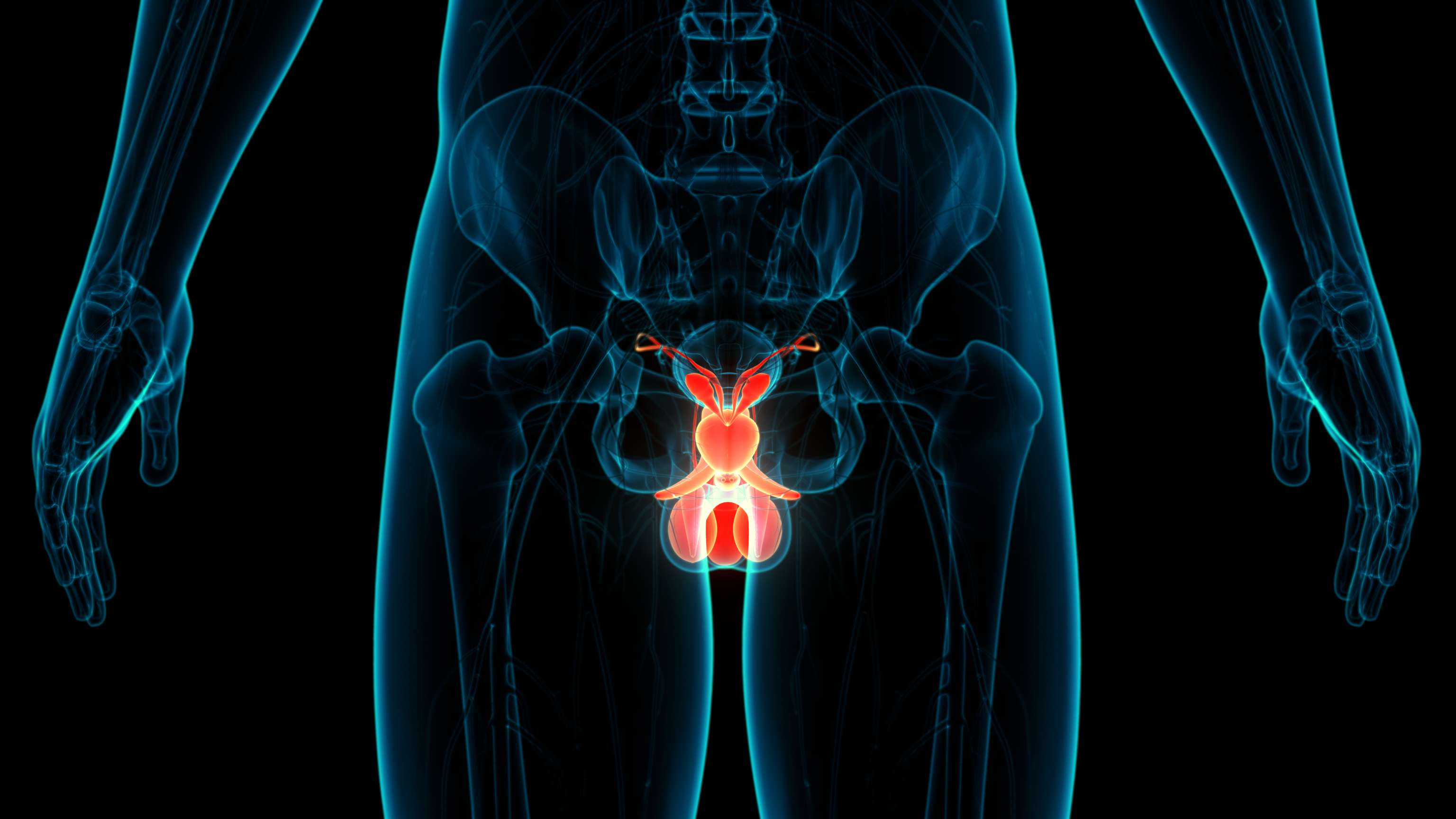
The term urethral stricture refers to a narrowing of the urethra. The medical term is derived from the Latin word "strictura", (engl.: to contract).
About 1% of the population suffers from urethral stricture, and about half of all cases are either medically caused or occur due to unknown causes (idiopathic). The incidence of urethral stricture increases significantly with age, rising to over 100 cases per 100,000 population in people over 65 years of age. It mainly affects men.
Depending on the severity and duration of symptoms, urethral stenosis can have long-term negative effects on the entire urinary tract. Urethral strictures cause continuous damage to the entire urinary tract due to functional obstruction. They can also lead to reduced kidney function if they progress chronically.
Although it is a common urological condition, there are no guidelines on urethral stricture from the European Association of Urology (EAU). Various treatment options are available depending on the anatomical location of the stricture. The treatment options for urethral stricture should always be selected after education and diagnosis by the treating physician. Likewise, the individual preferences of the affected person play a major role in the treatment decision.
Urethral stricture in women
In contrast to men, urethral stricture rarely occurs in women. In women, traumatic (e.g. after childbirth) or medically induced urethral strictures (e.g. after radiation) are usually in the foreground. However, the pathogenesis of this disease is not yet fully understood.