New findings in the treatment of migraines
Pathological mechanisms and causes of migraine
Migraines are attack-like chronic headaches that occur in episodes, which can be very severe and can often be characterized by accompanying symptoms. They are described as pulsating, throbbing or hammering and are usually located on one side of the head. Activity worsens the condition. Accompanying symptoms include nausea, vomiting, sensitivity to smells, photophobia, sensitivity to sound, tearing of the eyes or dizziness. An aura can also occur. This usually precedes the pain and can manifest itself in the form of seeing flashes of light (ciliated scotoma), speech or sensory disturbances.
The exact pathological mechanism has not yet been clarified. So far, there are only hypotheses that have not yet been fully verified. It is assumed that migraine is caused by an expansion of the blood vessels in the brain. This dilation (vasodilation) is caused by the trigeminovascular reflex, according to the theory. Pain receptors in the blood vessels cause irritation of the trigeminal nerve, which then causes the electrical impulses to spread through the cerebral cortex, resulting in the sensation of pain.

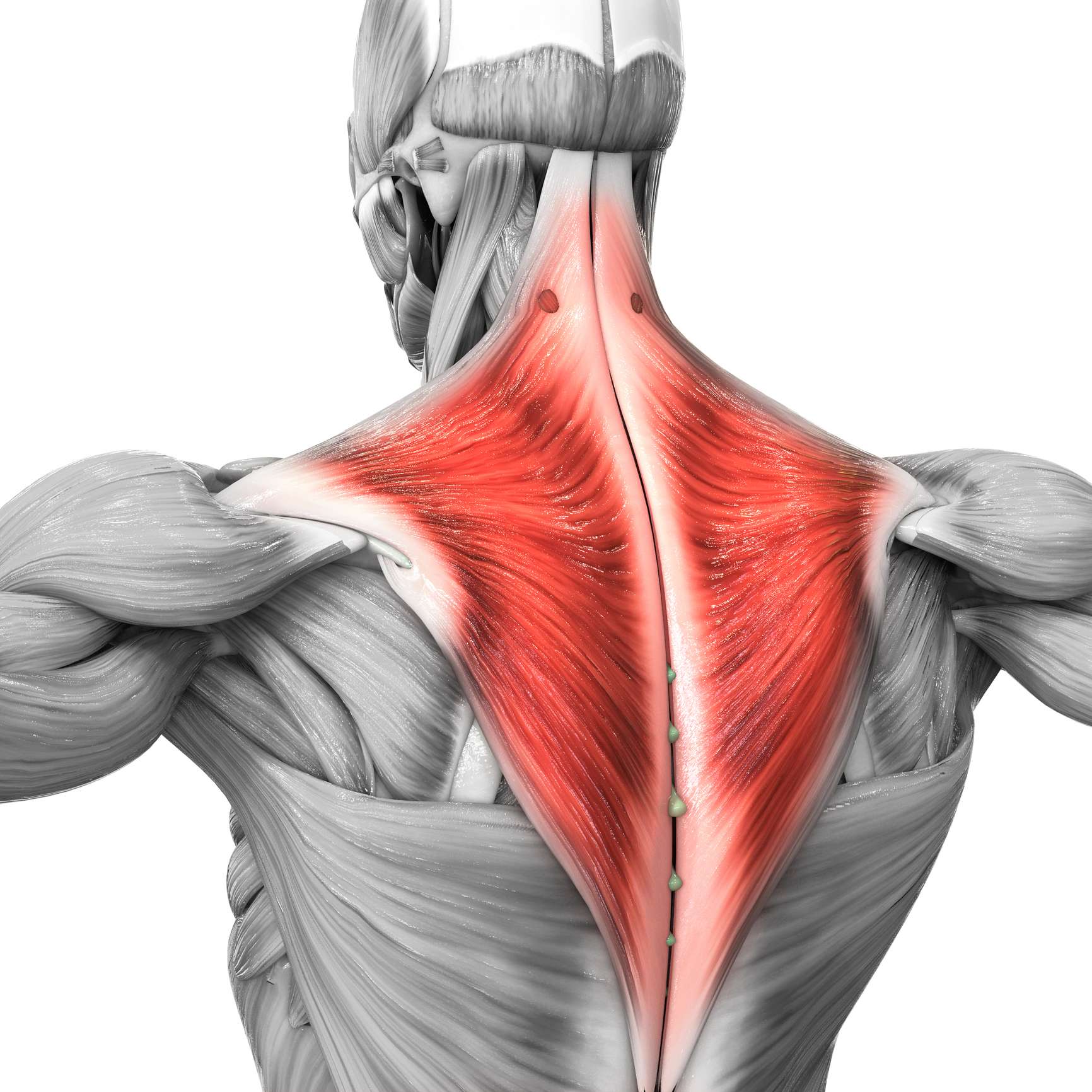
New cause discovered
A team of German researchers recently discovered a link between the trapezius muscle, the large muscle of the neck, and migraines. They found that there is an increase in inflammatory parameters in people with headaches. These small inflammations were visualized using MRI. A hyperintense signal in the T2 weighting is decisive for the diagnosis. The T2 weighting is a contrast display of the MRI image, where it is differentiated by the T2 relaxation time. If there is inflammation, this signal is recognizable. T2 was significantly higher in people with headaches compared to the control group. However, there was an even higher signal in test subjects with migraines. The research group also found that T2 correlates with the number of headache days. The greater the number, the greater the signal. The new finding could provide an approach for new therapeutic options in migraine treatment that could dispense with medication. Non-drug therapy would also eliminate the risk of side effects and interactions.
Migraine therapy
There are two different methods of treating migraines. The first is acute therapy, in which migraine attacks are treated. The second is prophylaxis, in which medication is used to try to reduce the number of headache days.
Acute therapy
Several classes of drugs are used in the acute treatment of migraine. The most effective is the triptan class. Triptans work by binding to the 1B and 1D subtypes of serotonin receptors. They cause vasoconstriction, which is intended to suppress the pain. Another group are the Gepante. They have an antagonistic effect on the CGRP receptor (calcitonin gene-related peptide). The activation (induction) of this receptor also causes vasodilation (vasodilation). Some other drug classes are also used for the acute treatment of migraine, but are not as effective as those described here. These include the ergot alkaloids and non-opioid analgesics. The ergot alkaloids are rarely prescribed as the side effect profile is usually very high and the effect is not as strong as that of the triptans. The non-opioid analgesics are the well-known painkillers such as ibuprofen, acetylsalicylic acid (aspirin), diclofenac and many more. The problem with this group is that they do not work well enough to adequately treat a moderate to severe migraine attack.
Prophylaxis
If the number of migraine attacks exceeds 15 headache days per month, prophylaxis can be considered. An attempt is made to reduce the number of attacks by means of medication. Most prophylactic drugs were not primarily developed for use in migraine treatment, but only proved to be effective later. Beta-blockers such as metoprolol, propranolol or bisoprolol are used here. These are actually intended as medication for the treatment of high blood pressure. They are generally taken in tablet form and are the active ingredient class of choice for prophylactic migraine treatment. Metoprolol and propranolol are the most effective. Although flunarizine is also a drug used to treat high blood pressure, it belongs to a different class of active ingredients and is the only member of this class that can be used to prevent migraines. Antiepileptic drugs such as topiramate or valproic acid can not only reduce the frequency of epileptic seizures, but also that of migraine attacks. However, it should be noted that these two agents are only used when beta-blockers are not an option, as antiepileptic drugs have a greater side effect profile. Pizotifen and methysergide work by inhibiting serotonin receptors, but are hardly used any more due to numerous severe side effects. CGRP inhibitors such as erenumab, fremanezumab or glacanezumab are monoclonal antibodies that can be extracted from animals, usually mice, processed and then administered. These are actually used in cancer therapy, but have also proven to be effective in migraine therapy. The disadvantage of these preparations, however, is that they have to be administered either into the subcutaneous fatty tissue or into the vein and must therefore be administered by trained personnel.

New active ingredient approved
In December 2022, new active ingredients for migraine treatment were approved. The most important discovery is that of lasmiditan. This new active ingredient has also led to the development of a new class of active ingredients, ditans. Lasmiditan is a new type of active ingredient for the acute treatment of migraines. Unlike the triptans, it acts on the 1F sub-receptor type, with the advantage that it cannot cause any side effects on the heart. The effect of lasmiditan is not fully understood, but it is assumed that it inhibits the release of neuropeptides that are responsible for the transmission of pain. However, Ditane is not the drug of choice. They should only be used if the triptan group is not effective or if there is a contraindication to taking triptans. The efficacy of lasmiditan has been confirmed in studies, but comparative studies with triptans are still pending.
Conclusion
As the number of migraine patients increases, so does the need for effective treatment options. Particularly in the case of migraine, not every preparation works the same for everyone and new treatment options must therefore be found. The new findings described in this article can contribute to better care for migraine patients and offer new hope for those for whom previous therapies have failed.
Sources
- DocCheck, M. B. (2005, Mai 16). Migräne. DocCheck Flexikon; DocCheck Community GmbH.
- DocCheck, M. B. (2010, Dezember 6). Myositis. DocCheck Flexikon; DocCheck Community GmbH.
- DocCheck, M. B. (2019, Juli 15). CGRP-Rezeptor. DocCheck Flexikon; DocCheck Community GmbH.
- Entwicklungsstufe:, S. (o. J.). Therapie der Migräneattacke und Prophylaxe der Migräne. Awmf.org.
- Europäischer Kopfschmerz- und Migränetag - ÖGN - Österreichische Gesellschaft für Neurologie. (o. J.). ÖGN - Österreichische Gesellschaft Für Neurologie.
- Lasmiditan. (o. J.). Chemspider.com.
- Öffentliches Gesundheitsportal Österreichs. (o. J.). Gesundheitsportal.
- PharmaWiki - Migräne. (o. J.). Pharmawiki.ch.
- Sollmann, N., Schandelmaier, P., Weidlich, D., Stelter, J., Joseph, G. B., Börner, C., Schramm, S., Beer, M., Zimmer, C., Landgraf, M. N., Heinen, F., Karampinos, D. C., Baum, T., & Bonfert, M. V. (2023). Headache frequency and neck pain are associated with trapezius muscle T2 in tension-type headache among young adults. The Journal of Headache and Pain, 24(1).
- Wikipedia contributors. (o. J.). Migräne. Wikipedia, The Free Encyclopedia.

Thomas Hofko
Last updated on 27.06.2024
Your personal medication assistant
Browse our extensive database of medications from A-Z, including effects, side effects, and dosage.
All active ingredients with their effects, applications, and side effects, as well as the medications they are contained in.
Symptoms, causes, and treatments for common diseases and injuries.
The presented content does not replace the original package insert of the medication, especially regarding the dosage and effects of individual products. We cannot assume liability for the accuracy of the data, as the data has been partially converted automatically. Always consult a doctor for diagnoses and other health-related questions.
© medikamio