Basics
Gastritis, also called gastric mucosa inflammation, is an inflammation-related damage of the gastric mucosa(lat. Tunica mucosa gastrica). Depending on the variation, superficial to deeper changes in the glandular tissue may occur.
Gastritis, also called gastric mucosa inflammation, is an inflammation-related damage of the gastric mucosa(lat. Tunica mucosa gastrica). Depending on the variation, superficial to deeper changes in the glandular tissue may occur.
Depending on the course of the disease, a distinction is made between acute and chronic gastritis. The latter usually develops gradually and sometimes manifests itself late with rather unspecific symptoms. Chronic gastritis is basically divided into three types, which are distinguished by different causes.
Type A - Autoimmune gastritis | |
Origin | In autoimmune diseases, the human immune system produces antibodies against the body's own cells or cell components. In the case of autoimmune gastritis, antibodies against an acid-forming protein (H+/K+-ATPase) of the gastric vestibular cells and/or intrinsic factor are known. Stomach cells are cells in the gastric mucosa that are responsible for the production of hydrochloric acid (a component of gastric juice, HCl) and intrinsic factor (a protein for the absorption of vitamin B12 in the small intestine). The inflammation caused by the autoantibodies leads to the death of the gastric mucosa cells and to the atrophy of the gastric mucosa. The development of type A gastritis may also involve Helicobacter pylori bacteria, which are otherwise associated with type B gastritis. |
Frequency | Autoimmune gastritis is the rarest form of chronic gastritis, accounting for 3-6% of all cases. It may have a hereditary component and affects almost exclusively Northern Europeans or Scandinavians. |
Type B - Bacterial gastritis | |
Origin | Type B gastritis is caused by the bacterium Helicobacter pylori, which is transmitted from person to person. |
Frequency | Type B gastritis accounts for about 80-90% of all chronic gastritis and is the most common subtype. The number of people affected increases correlatively with age, as H. pylori contamination increases. There is hardly any disease below the age of 20. |
Type C - Chemical gastritis | |
Origin | Type C gastritis is caused by a chemical-reactive irritation of the stomach. This can be caused, for example, by non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, acetylsalicylic acid, naproxen or diclofenac. Their use inhibits the formation of the tissue hormone prostaglandin, which is responsible for the formation of gastric mucus and gastric acid neutralizing substances. Other substances such as nicotine and alcohol and, in rarer cases, reflux (backflow) of bile can also be responsible for type C gastritis. |
Frequency | About 10-15% of all chronic gastritis cases are chemical gastritis. |
Chronic inflammation of the gastric mucosa often causes no or uncharacteristic gastrointestinal symptoms. Acute gastritis with corresponding symptoms is possible in the setting of chronic gastritis.
Type A |
|
Type B | Type B gastritis does not cause specific symptoms. However, there is an increased risk for:
|
Type C | This type of gastritis also shows only non-specific sypmtoms, which are similar to those of acute gastritis. Possible complications are gastric bleeding and ulcers. |
Type A | A way to treat the cause of autoimmune gastritis does not yet exist. In case of an existing vitamin B12 deficiency, a (often lifelong) substitution of the vitamin is carried out. If H. pylori is detected, it should be eradicated (see below). | ||||
Type B | The first priority in bacterial gastritis is the eradication of Helicobacter pylori. For this purpose, there are different therapy regimens which are selected according to the resistance situation and individual factors:
If therapies are unsuccessful, testing for antibiotic resistance should be performed. | ||||
Type C |
|
All recommendations that apply to acute gastritis can also alleviate the symptoms of chronic gastritis. These include a light diet, avoidance of coffee, alcohol and nicotine, stress reduction and adequate fluid intake.
Chronic gastritis can last from several weeks to years. Depending on the cause, chronic gastritis can also heal without complications.
What the prognosis is depends on the type of gastritis:
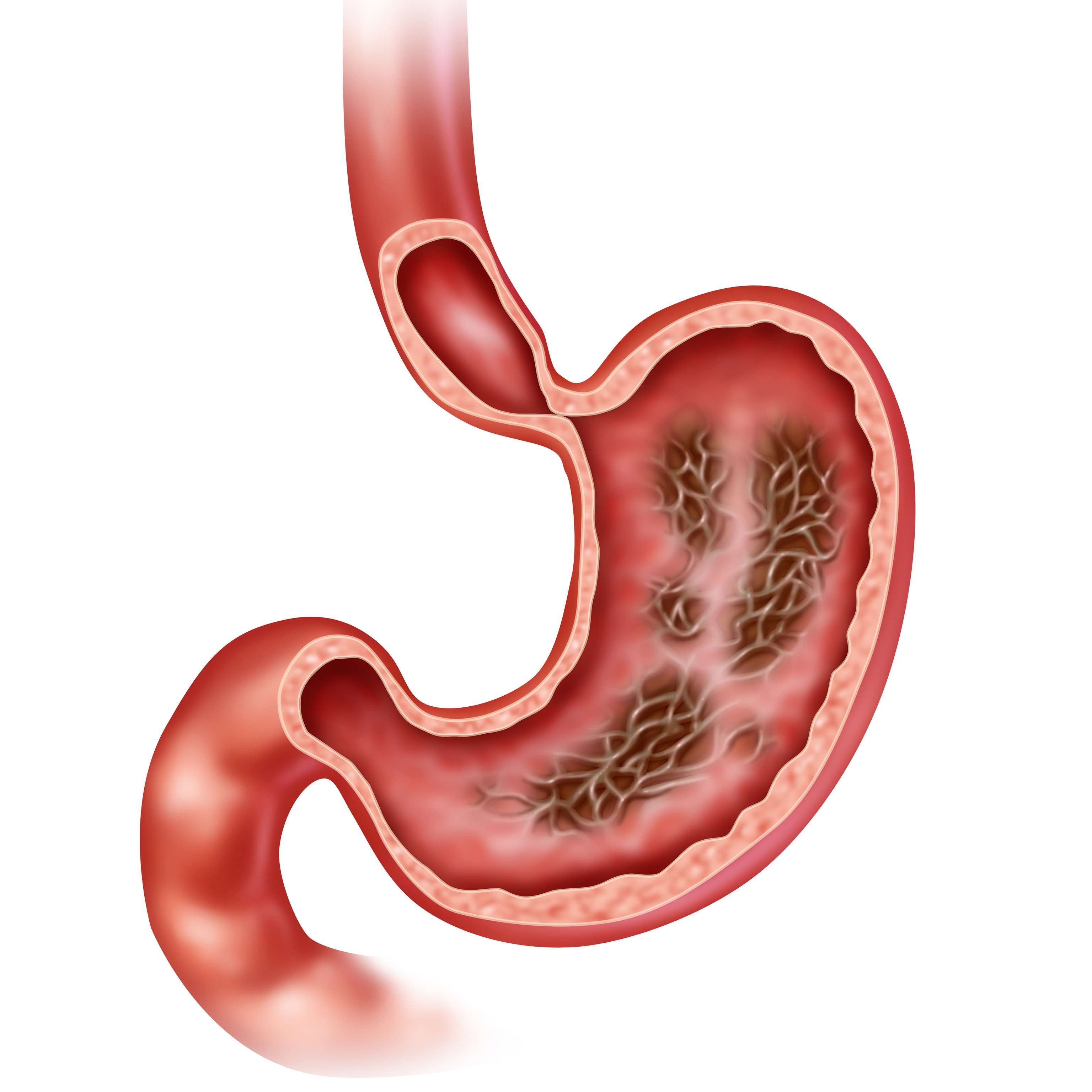
Erosions (superficial defects of the gastric mucosa with intact gastric wall) in acute or chronic form are also possible. They are the symptom of various damages or diseases, but the exact cause usually remains undiscovered.
In order to detect and treat gastric carcinomas at an early stage, regular gastroscopy is recommended in cases of chronic gastritis.
A generally conscious approach to alcohol, nicotine and painkillers reduces the risk of developing chronic gastritis.
If painkillers are taken over a long period of time, it is recommended that patients at risk take a proton pump inhibitor (PPI) at the same time.

Olivia Malvani, BSc

Dr. med. univ. Bernhard Peuker, MSc
Browse our extensive database of medications from A-Z, including effects, side effects, and dosage.
All active ingredients with their effects, applications, and side effects, as well as the medications they are contained in.
Symptoms, causes, and treatments for common diseases and injuries.
The presented content does not replace the original package insert of the medication, especially regarding the dosage and effects of individual products. We cannot assume liability for the accuracy of the data, as the data has been partially converted automatically. Always consult a doctor for diagnoses and other health-related questions.
© medikamio